How to Read a Monitor at a Hospital
It'south your first day equally a clerk in the Emergency Department and your staff has asked you to run across an 80 year one-time patient with known COPD presenting with increasing shortness of breath. He reminds y'all to check the patient monitor when y'all go in there to wait for any abnormalities and to record a new set of vitals on the chart.
Patient monitors can be overwhelming early in your training when you're non quite certain what you're looking at. There are and then many numbers, waveforms, and sounds – how are y'all supposed to know what is what? When you're in a busy Emergency Department, it is important to be familiar with what a typical patient monitor looks similar and how to interpret all of the components. Knowing the nuts of patient monitor interpretation and ECG pb placement can make a junior clerk a valuable fellow member of the Emergency Department team.
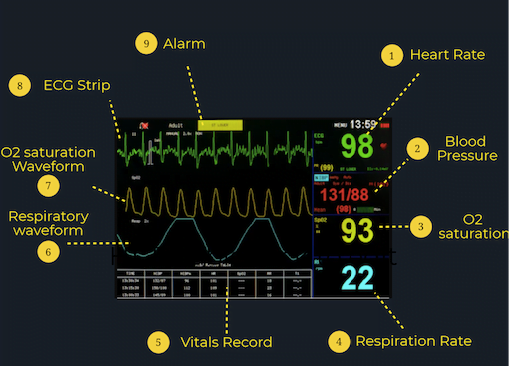
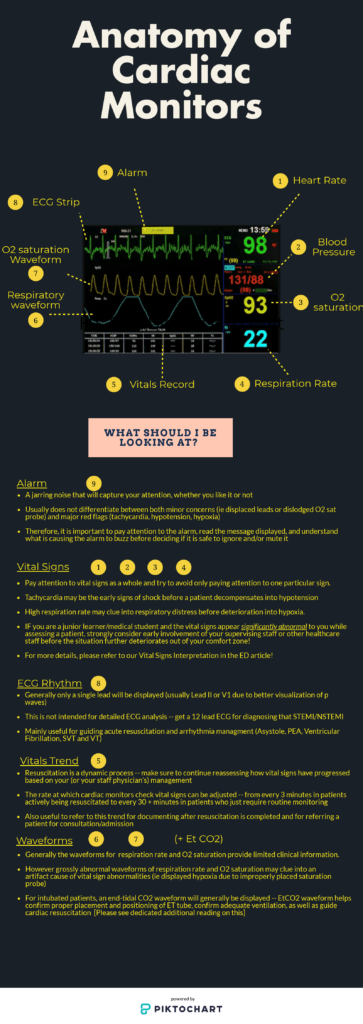
Here is an case of a patient monitor. The typical layout includes the numerical vital signs on the right and the waveforms on the left, giving you a general overview of the patient's real-time vitals.
What the Numbers Mean:
Various patient monitors can record and track a wide array of data, but almost all patient monitors will record these fundamental vital signs:
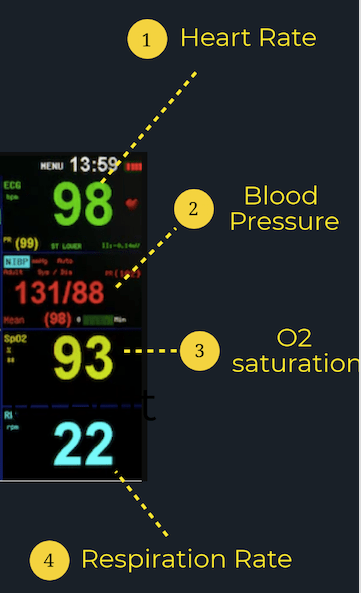
Eye Rate (HR): Typically, the heart charge per unit is presented at the height of the monitor in green. The number volition exist identified by a "HR" or "PR" (pulse rate) beside or merely higher up it and is presented in beats per minute (bpm). A normal developed has a resting heart rate between threescore-100 bpm.
Blood Force per unit area (BP): The patient's blood pressure is typically presented on the screen under "SYST" or "SYS" for systolic and "DIAS" or "DIA" for diastolic. An average BP is around 120/80.
Oxygen Saturation (SpO2): The patient's oxygen saturation will be located on the monitor nether "SpO2" and is a mensurate of the corporeality of oxygen in the patient's blood. A normal O2 saturation is 95% or greater; however, it is important to retrieve that some populations such as those with COPD take a lower normal cutoff.
Respiratory Rate (RR): Look for the patient'due south respiratory rate under "RR" on the patient monitor. It is reported in breaths per minute, with normal values betwixt 12 and 20. Nevertheless, this number isn't very accurate, peculiarly as the patient's breathing goes faster or slower.
What the Lines Mean:
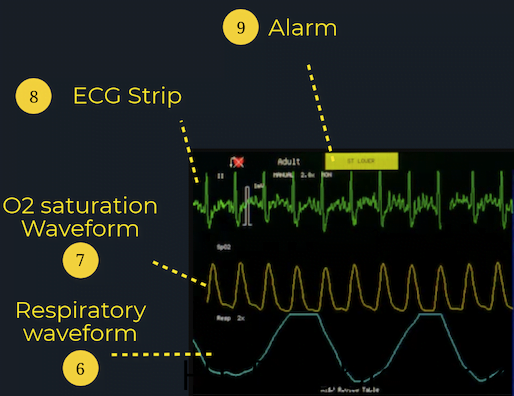
ECG Readout:The ECG readout on the patient monitor is non intended for detailed ECG analysis every bit information technology typically but represents 1 lead (most normally atomic number 82 II). Instead, it is near useful for guiding acute resuscitations or managing arrhythmias, since it can requite you lot some information on the electric activeness of the heart and its level of function. If you have any concerns regarding a patient's cardiac office, get a 12-lead ECG! Knowing the proper lead placements for five-signal cardiac monitors and 12-atomic number 82 ECGs is likewise an important skill for junior learners in the ED. For resources to review lead placements, check out the CanadiEM Frontline Primer or this blogpost by Life in the Fast Lane for an in-depth explanation.
SpO2 Waveform: The SpO2 waveform allows clinicians to make up one's mind whether there are any bug with apportionment or peripheral perfusion. Each peak of the SpO2 waveform should correlate with a heartbeat on the ECG waveform at the same intervals, since oxygenated claret is beingness pumped out of the heart with each heartbeat.
Respiratory Waveform: The "RESP" waveform on the monitor is useful for clinicians to monitor for any respiratory issues such every bit apnea or dyspnea.
What the Alarm Means:
If whatever of the vital signs fall outside of the range of normal, the patient monitor will alert clinicians past sounding an warning and flashing an alarm on the screen. Although the alert may indicate a serious event such as a sudden drop in O2 saturation or BP, it is important to notation that just because the alarm is going off doesn't ever hateful that there is a clinical problem. I of the most common reasons for the alarm to go off is considering one of the sensors isn't receiving information. The screen may show no reading, a fluctuating numerical value or waveform, or a reading that does not represent with the clinical film. Always brand sure that all of the wires and probes are properly attached and secured! Information technology'due south also common for the alarm to suggest Vfib but the patient could merely be moving (or seizing). Nevertheless, if you are ever concerned with the values or readouts that are being presented on the patient monitor, bank check your patient and find your senior resident or staff as soon every bit possible. It'due south amend to exist safe than sorry!
Lastly, junior learners sometimes make the error of focusing too much on one abnormal number. If ane vital sign lies outside of the normal limits, this may bespeak a trouble; however, information technology could also exist an outlier. Retrieve that a patient's Hr may be elevated due to pain, white glaze syndrome, or potent emotions. Similarly, a BP may modify due to the patient's position or hydration status. As a upshot, it is important to remember to always interpret the vital signs together and in the context of the patient's clinical movie and consider many possible explanations for why the vitals are aberrant.
Download this infographic to keep with you in the ED or on the wards for a quick refresher on the go!
Reviewing with the Staff
I take a love/hate human relationship with the monitor. I recall as a junior medical student my first day on pediatrics when I was caring for a vi month sometime boy. During my rounds, the monitor all of a sudden started alarming. His heart rate was 140! My expression frightened his mom and she and I rushed outside to take hold of the nurses and a pediatrician. Turns out 140 is only the upper limit of characters for tweets and is perfectly normal for that age range. I was led astray by that monitor and information technology spawned a decade long feud.
Now I've come to appreciate it a niggling more; with familiarity I've learned that the alarms are a reminder for y'all to cheque the patient. Remember any number that doesn't fit with what you're seeing needs further investigation. The automatic BP tin exist influenced past a number of factors, but sometimes that single low reading might be a message. I had a 80 yo male with one reading of 60/40 and then every subsequent reading was 120/80. He ended up passing from a ruptured abdominal aneurysm within 30 minutes. Other times the reading could be completely spurious so watch out for trends.
The respiratory rate is on the whole, unreliable. Always measure RR manually as information technology is the most sensitive indicator of illness and the motorcar measurement is usually wrong (unless we're talking about a patient on a ventilator).
The bedside nurses are a great resource on monitors - they accept a ton of tricks to setup, translate and change the monitor and I'd encourage you to ask them to share their knowledge. Remember, many hospitals have varied setups then although they basically do the aforementioned thing the menus and setup are probable different.
1 pro tip I learned from my nursing colleagues is that you tin can adjust the EKG monitor to slow downwardly the charge per unit, this stretches out your EKG and tin help distinguish faster rhythms - it can aid pull out the sawtooths of atrial palpitate. It tin can aid distinguish SVT vs Sinus tach. Spend time with the monitor and it volition give you its secrets.

Dr. Alim Nagji
Alim Nagji is an ER staff at Joseph Brant (JBH) & St. Joseph Healthcare Hamilton. He is the Manager of Emergency Medicine Clerkship for McMaster Academy and the Manager of Simulation Learning and Clinical Pedagogy Unit for JBH. He has interests in medical education, simulation and global health. Send him your favourite meme on twitter @alimnagji
(Visited 188,875 times, 7 visits today)
callawaysonts1966.blogspot.com
Source: https://canadiem.org/how-to-read-patient-monitors/

0 Response to "How to Read a Monitor at a Hospital"
Post a Comment